Mar 20, 2024, 4:00 am UTC
5 min
Created by
An often-missed disease in women increases the risk of dementia
Microvascular disease impacts the tiniest blood vessels—arterioles, capillaries, venules—in the body. Women are more prone to developing this systemic disease, and emerging research suggests it could be contributing to their higher risk of dementia.
The human body is like a finely tuned engine, with every organ and tissue intricately linked by a network of blood vessels, much like the infrastructure that connects the essential components of a high-performance machine. Within this vast circulatory system, arterioles, capillaries, and venules act as narrow pathways that branch off larger arteries and guarantee that oxygen, nutrients, and other essential supplies reach even the most remote cells and tissues. However, when these minuscule vessels become dysfunctional—a condition known as microvascular dysfunction—the consequences ripple beyond their small scale, affecting virtually every bodily function.
For decades, microvascular dysfunction in the heart, which predominately affects women, has been disregarded, understudied, and underdiagnosed. But, in recent years, scientists have uncovered a compelling correlation that has catapulted it into the spotlight: people with coronary microvascular dysfunction face an elevated risk of developing dementia.
Now, a collaborative effort between cardiologists and neurologists at Rush University Medical Center in Chicago seeks to investigate this heart-brain link with the aim of empowering patients to take their brain health to heart.
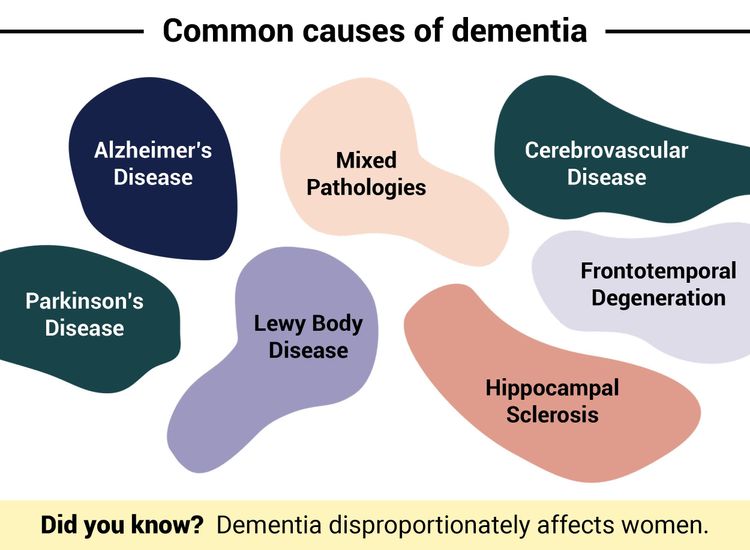
 Infographic by Cat Lau. (References below)
Infographic by Cat Lau. (References below)
What is microvascular dysfunction?
Microvascular dysfunction, also known as "small vessel disease," describes the abnormal expansion or constriction of tiny blood vessels throughout the body. When these micro-vessels—which are crucial for regulating blood flow—malfunction, they can lead to organ failure, tissue damage, chronic pain, and neuropathy, among other health complications.
While this dysfunction can affect any organ system, one common type—coronary microvascular dysfunction (CMD)—impacts the small vessels supplying blood to and from the heart muscle. Unlike other heart diseases, where plaque buildup in the larger coronary arteries restricts blood flow, CMD is caused by trauma to the micro-vessels within the heart itself.
Yet, the condition is nearly indistinguishable from other heart diseases because it mimics their symptoms—including shortness of breath, fatigue, and chest pain. It is also hard to diagnose because the affected blood vessels are less than a millimeter in diameter, which renders them undetectable using standard diagnostic tests like angiograms.
How does microvascular dysfunction affect the brain?
Today, almost two-thirds of people living with the most common form of dementia—Alzheimer's disease—are women. Similarly, women are disproportionately affected by cardiovascular diseases that involve impaired function of micro-vessels, with studies suggesting they make up as much as 80% of all cases.
Women with microvascular dysfunction also face worse outcomes compared to men, in part because knowledge of this condition has historically relied upon male-centric data. Furthermore, it wasn't until recently that medical professionals realized that even in the absence of traditional blockages in the larger arteries, dysfunction may still affect blood flow in the smaller ones.
So what's the connection between the heart and the brain? Research suggests that the heart and the brain have similar blood vessel setups: larger arteries spreading across their surfaces, which then branch into tiny penetrating vessels that supply blood to the organs through a microscopic network. Similarly, the mechanisms and risk factors for coronary microvascular dysfunction also contribute to small vessel disease in the brain. In fact, 45% of dementias are caused by the malfunction of these small, brain-infiltrating vessels.
45% of dementias are caused by the malfunction of small blood vessels in the brain
Now, new research is linking cardiovascular diseases to the start and progression of Alzheimer's disease.
"We know that nearly 80% of people with Alzheimer's have heart disease, and studies have also found small-vessel disease in the brains of many of these patients," says Dr. Annabelle Volgman, a nationally recognized cardiologist, who is also the co-founder and medical director of the Rush Heart Center for Women in Chicago, who was not involved in this particular study. "This means something's happening in both the hearts and the brains of people with cardiovascular disease and Alzheimer's. And microvascular dysfunction seems to be the obvious link between the two."
Symptoms of small-vessel disease in the brain
1. Strokes
2. Cognitive decline and brain fog
4. Motor challenges
5. Slurred speech
6. Depression
7. Fatigue
Source:
How does microvascular dysfunction elevate dementia risk?
According to Volgman, the malfunction of small blood vessels can worsen processes that lead to dementia. This includes problems with the brain's protective barrier, reduced blood flow to the organ, and inflammation:
Cerebral Blood Flow (CBF) regulation: The brain relies on a steady supply of oxygen and nutrients delivered through cerebral blood flow. This delivery is tightly regulated to match the brain's metabolic demands. Small blood vessels, including arterioles and capillaries, regulate cerebral blood flow. However, when these vessels malfunction, it can disrupt blood flow regulation. Microvascular dysfunction can also result in reduced blood flow to specific brain regions, a condition known as cerebral hypoperfusion. Chronic cerebral hypoperfusion has been linked to abnormal neuron function, deterioration of synaptic connections between neurons, and neurodegeneration — hallmark features of Alzheimer's disease.
Blood-Brain Barrier (BBB) integrity: The blood-brain barrier is like a protective shield of cells lining the brain's blood vessels. It carefully controls what moves between the bloodstream and the brain, shielding the brain from harmful substances while letting essential nutrients through. However, microvascular dysfunction can disrupt this barrier, causing leakage of red blood cells and proteins into the brain. This typically triggers an inflammatory response within the brain, leading to neural damage.
Neuroinflammation: Microvascular dysfunction sets off a chain of events that triggers inflammation and oxidative stress. In response to infections or tissue damage, immune cells like macrophages and neutrophils produce reactive oxygen species (ROS) and inflammatory proteins called cytokines to fight off pathogens or to repair damaged cells. However, if their production goes unchecked, it can cause oxidative stress, which harms nearby tissues and worsens inflammation. Microglia—the brain's resident immune cells—also become active in response to tissue damage or inflammation signals. Microvascular dysfunction can lead to prolonged activation of microglia, which contributes to chronic inflammation.
Chronic inflammation in the brain can have wide-ranging effects on brain function due to damage and degeneration of neurons. This ultimately contributes to the progression of neurodegenerative diseases like Alzheimer's.
Amyloid beta (Aβ) clearance: Alzheimer's disease is characterized by the buildup of amyloid beta protein in the brain. Microvascular dysfunction can interfere with the body's ability to clear Aβ from the brain and even encourage its buildup as a result of irregularities in cerebral blood flow, damage to the blood-brain barrier, and chronic neuroinflammation.
How are researchers harnessing this heart-brain link to understand and lower the risk of dementia?
The Cardiology Cognitive Clinic at Rush is one of a kind, where heart experts like Volgman collaborate with neurologists to understand and treat heart disease in women and find ways to prevent cognitive decline and dementia. "We're a group of people who are passionate about this heart-brain link, but it's not in the mainstream — most cardiologists are certainly not focused on cognitive behavior," Volgman explains.
Volgman and her Rush colleague, neurologist Neelam Aggarwal, are analyzing data from a study that looks at cognitive decline in women with cardiovascular disease and whether certain activities that lower the risk of heart disease can also help slow cognitive decline. As part of this study, the researchers assigned 250 women to different groups based on interventions — brain games, computer games, physical activity, a combination of physical activity and brain games, or just continuing with their normal routine, as the placebo.
The findings will give them a better understanding of the relationship between cardiovascular health, and cognitive decline and Alzheimer's. In the meantime, the collaboration has made one thing clear: that "the brain is exposed to everything the cardiovascular system brings it," says Volgman. "So, whatever we do to the heart, we're doing to the brain."
Infographic references
- Women and Coronary Microvascular Dysfunction (CMD), Go Red for Women (Accessed March 13, 2024)
- Why women's heart health? Canadian Women's Heart Health Alliance (Accessed March 13, 2024)
- Paolini Paoletti F, Simoni S, Parnetti L, Gaetani L. The Contribution of Small Vessel Disease to Neurodegeneration: Focus on Alzheimer's Disease, Parkinson's Disease and Multiple Sclerosis. Int J Mol Sci. 2021 May 7;22(9):4958.
- Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 2019 Jul;18(7):684-696.
- Kempuraj D, Thangavel R, Selvakumar GP, Zaheer S, Ahmed ME, Raikwar SP, Zahoor H, Saeed D, Natteru PA, Iyer S, Zaheer A. Brain and Peripheral Atypical Inflammatory Mediators Potentiate Neuroinflammation and Neurodegeneration. Front Cell Neurosci. 2017 Jul 24;11:216.
- Having ideal heart health may lessen the risk for brain vessel disease. American Heart Association. (Accessed March 13, 2024)