Dec 20, 2023, 5:00 am UTC
4 min
Created by
Estrogen and the Brain: New clues about dementia risk in women
Estrogen, the female sex hormone produced mainly in the ovaries, has a powerful effect on the brain across a woman's lifespan. As a master regulator, it is known for influencing a woman's appetite, mood, and sleep. It also controls the body's energy balance and metabolism. So, what happens in the brain when estrogen levels begin to wane in midlife?
Many of the changes experienced by females in the years leading up to menopause — hot flashes, fatigue, irritability — are brought on by fluctuating levels of estrogen. In fact, a whopping 80 percent of women experience these kinds of brain-related symptoms in midlife.
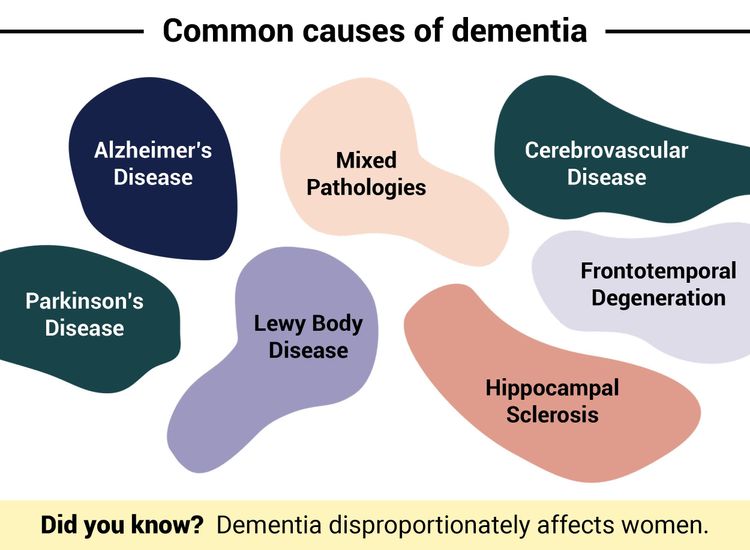
But the brain effects of falling hormone levels go much further. Low estrogen increases the risk of dementia and may help explain why two-thirds of people with Alzheimer's in the U.S., the most common type of dementia, are female. It may also heighten the risk of other neurodegenerative diseases, hasten their progression, or increase the level of disability associated with chronic conditions like multiple sclerosis.
So, what do we know about the brain changes that occur during the menopause transition and beyond? And what's the connection between estrogen and dementia?
 Infographic by Cat Lau. (References below.)
Infographic by Cat Lau. (References below.) How do low levels of estrogen affect the brain during menopause?
The road to menopause is rocky for most women. This stage of a female's life is marked by a diminishing supply of mature eggs in the ovaries, irregular ovulation, decreasing levels of sex hormones estrogen and progesterone, and an array of unwanted symptoms.
What is menopause?
Menopause is defined as one year after your last period.
What is perimenopause, or the “menopause transition”?
Perimenopause is the time leading up to menopause, when hormones start to fluctuate and then decline.
While many of these symptoms are associated with changes in ovarian function, research suggests menopause is a neurological transition that rewires the brain. Many of its symptoms are, in fact, a result of these brain changes.
Estrogen, for example, influences the activity of chemical messengers that mediate communication between neurons. When estrogen levels are low, estrogen receptors in the region of the brain called the hypothalamus, which regulates body temperature, do not activate correctly, resulting in hot flashes and night sweats.
Other hallmark symptoms of menopause, like brain fog and forgetfulness, are also tied to the effects of estrogen on the brain. The hormone is vital for making and breaking connections, called synapses, between neurons. These synapses allow us to learn, adapt, and perform various cognitive functions. A decline in estrogen levels can slowly erode these connections and make them more susceptible to damage from stress and injury.
Signs of neurological changes in menopause
- Hot flashes
- Mood changes, such as increased irritability
- Brain fog
- Migraines
- Insomnia
- Anxiety
- Depression
Source: National Institute on Aging
Estrogen also regulates glucose, the brain's primary food source and the fuel for cognitive processes like memory and attention. A recent brain imaging study showed a significant drop in brain energy after menopause that impacts body, temperature, mood, sleep — and cognitive performance. (The good news is that the study also showed that in most women the brain adjusts to waning estrogen levels over time, recovering its form and function.)
The amygdala, the emotional processing center of the brain, isn’t shielded from the effects of fluctuating levels of estrogen either. Activation of estrogen receptors in the amygdala can reduce anxiety and stress, but when estrogen levels decline during menopause, it can lead to changes in emotional processing, such as mood swings, heightened stress response, and even depression.
Does a decline in estrogen levels after menopause increase a woman’s risk of neurodegenerative diseases like Alzheimer’s?
Recent research is adding to the evidence that estrogen protects against dementia, demonstrating that the higher a female's lifetime exposure to estrogen, the lower the risk of dementia. The age at which a person reaches menopause and other reproductive milestones like number of pregnancies, reproductive lifespan, and hormone therapy influence lifetime exposure to the hormone.
For example, in a newly published study, researchers found that females who experienced natural early menopause (before age 45) were at a higher risk of developing dementia, compared to those who entered natural late menopause, around age 55. (In the U.S., the average age of menopause is 51.)
These findings, according to the researchers, demonstrate that there's a potential link between the age of menopause and dementia risk. Still, many other factors like age, income level, and leisure activities also seem to play a role in a woman's overall risk of dementia. This means there's a need to further tease out the specific role of estrogen in dementia risk.
In another recent study, a meta-analysis combining the results of six clinical trials and 45 observational studies, researchers at Weill Cornell Medicine and their colleagues found that women who took estrogen to treat menopause symptoms during midlife were less likely to develop dementia than those who didn't.
While this analysis, encompassing more than 6 million women, demonstrates estrogen's protective effect on the brain, there's still a lack of conclusive data on whether replacing estrogen could reduce a woman's risk of developing Alzheimer's, primarily because estrogen levels start to decline in midlife while the onset of Alzheimer's is often observed decades later.
What is clear is that more research on the relationship between estrogen, hormone replacement therapy, brain health, and dementia risk is needed. Fortunately, in an ongoing clinical trial, the Weill Cornell researchers are hoping to collect more data on whether estrogen therapy in midlife influences the earliest signs of Alzheimer’s in women.
Infographic References
- How menopause reshapes the brain. Nature News. (Accessed December 15, 2023)
- Lephart ED, Naftolin F. Menopause and the Skin: Old Favorites and New Innovations in Cosmeceuticals for Estrogen-Deficient Skin. Dermatol Ther (Heidelb). 2021 Feb;11(1):53-69.
- Rehbein E, Hornung J, Sundström Poromaa I, Derntl B. Shaping of the Female Human Brain by Sex Hormones: A Review. Neuroendocrinology. 2021;111(3):183-206.
- Calvo N, Einstein G. Steroid hormones: risk and resilience in women's Alzheimer disease. Front Aging Neurosci. 2023 Jun 16;15:1159435.