This article covers:
- What is "mommy brain"?
- What is the history of the term "mommy brain"?
- How does the brain change during the perinatal period?
- How does the brain change in postpartum depression?
- What are the risk factors for postpartum depression?
- How does the newly approved drug for postpartum depression work?
The terms "mom brain," "momnesia," and "pregnancy brain" have something in common — they stereotypically label new mothers' brains as slow, forgetful, and inadequate.
Jodi Pawluski, a Canadian neuroscientist and researcher at the University of Rennes in France, has studied mothers' brains for decades, and she says it's high time we rebrand this concept.
In an interview with wmnHealth, Pawluski shares insights from her book, "Mommy Brain: Discover the amazing power of the maternal brain," newly published in English, to explain how women's brains adapt and remodel in powerful ways during pregnancy and the postpartum period, preparing them for parenting.
This interview has been lightly edited for breadth and clarity.
wmnHealth: What led you to write "Mommy Brain," and why do you think it's a valuable resource for parents?
 Jodi Pawluski: I've been studying the maternal brain for several years, and in 2017, my colleagues and I wrote a review article on how the brain changes with perinatal mental illness, specifically postpartum depression and anxiety. When we looked at the scientific literature, there were maybe 25 articles that had done some imaging on women's brains in relation to mood or anxiety symptoms and mental illness during the postpartum period. That was a big shocker for us — how little we know about the maternal brain when it comes to mental illness. Yet, the perinatal period is a very plastic time in the adult life. We also know that the number of parents that will struggle with mental illness during that time is roughly 1 in 5.
Jodi Pawluski: I've been studying the maternal brain for several years, and in 2017, my colleagues and I wrote a review article on how the brain changes with perinatal mental illness, specifically postpartum depression and anxiety. When we looked at the scientific literature, there were maybe 25 articles that had done some imaging on women's brains in relation to mood or anxiety symptoms and mental illness during the postpartum period. That was a big shocker for us — how little we know about the maternal brain when it comes to mental illness. Yet, the perinatal period is a very plastic time in the adult life. We also know that the number of parents that will struggle with mental illness during that time is roughly 1 in 5.
I think people really find comfort in knowing that the brain goes through a normal transition during pregnancy and the postpartum period. This is something that has motivated me to share the research in this area because it can give some calm to new parents. But, at the same time, it's also been important for me to highlight that we aren't studying the biology of these perinatal mental illnesses enough to have many answers.
Size-mic shift
Experts often look at brain size as indicative of “brain reserve,”which refers to the ability of the brain to deal with changes that come with normal aging, such as shrinkage of areas that contain nerve fibers. Research suggests the shrinkage of parts of the brain in pregnancy could be the result of “fine tuning” nerve cell connections, which makes mothers’ brains more efficient and specialized for parenthood. Brain size has no correlation with intelligence.
The term "mommy brain" has received quite a bit of scrutiny recently, and it's also the title of your book. Could you dive into its history?
Pawluski: When we use the term "mommy brain," it refers to a deficit — the idea that there's confusion and fogginess, and our brain is not functioning as expected. And, in doing so, we forget the importance of caregiving itself and that our brain is adapting to this essential activity. We have this negative narrative when it comes to motherhood and the brain. I want this story to change and for us to remember that our brain is doing amazing things as parents. More broadly, as a society, we need to think about how we can value parents and support them in ways that work best for them.
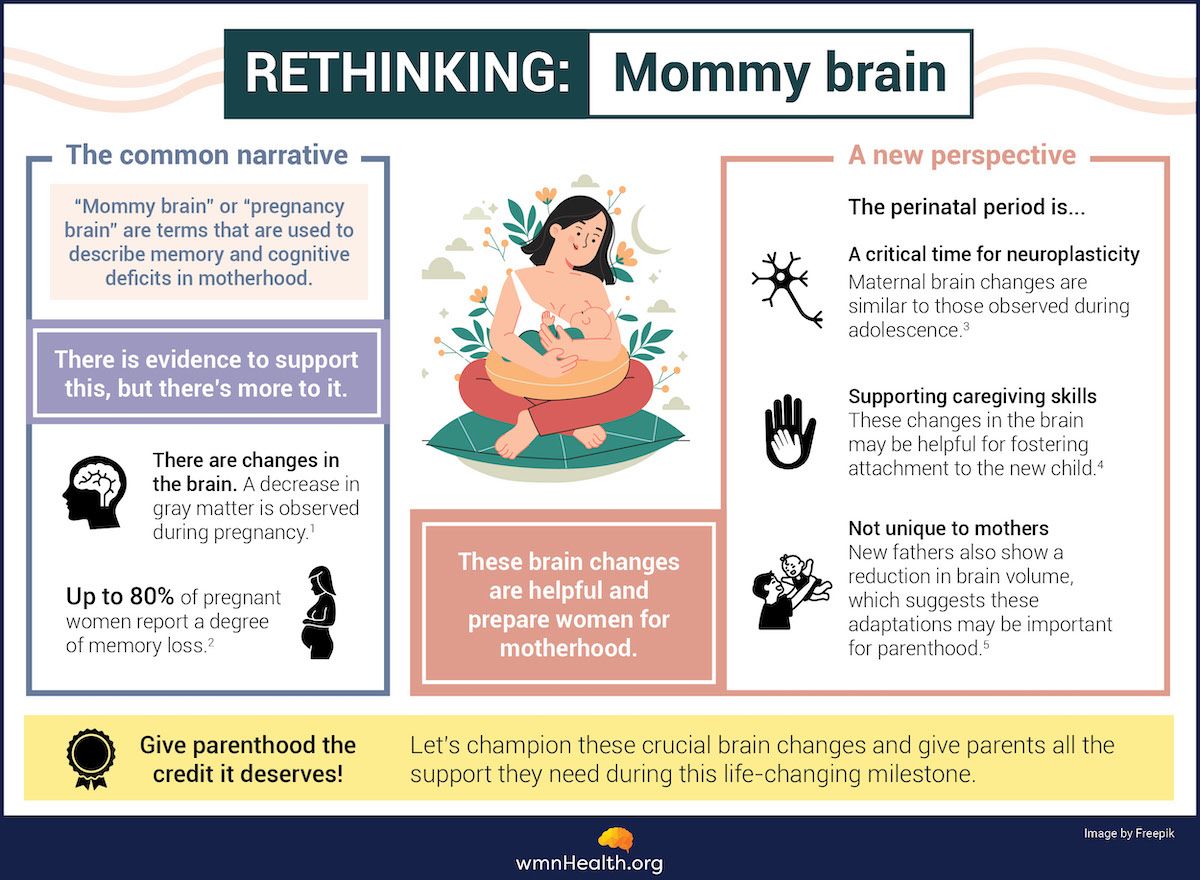
(Infographic references at the bottom of the article)
When you talk about brain changes from pregnancy to postpartum, what do these changes look like?
Pawluski: Over the past four decades or so, scientists have done a lot more research in animal models, where we can look at changes at the cellular level, at the receptors and neurotransmitters in the brain. But what we've seen in the popular press over the past few years is a focus on human research, where scientists usually look at things like the structure or size of the brain and the function or activity of the brain.
This research has really clarified that across pregnancy, there seems to be a decrease in the size of different brain regions, such as the amygdala and the prefrontal cortex, by about 1%. These areas of the brain are responsible for motivation, reward, emotional regulation, and decision-making, and they work together to coordinate responding to a baby. An increase in function in these areas results in a decrease in structure, and it's positively associated with feelings of attachment or sensitivity toward the baby. The brain may be slightly smaller but more powerful, like dynamite in small packages.
What you just described are some of the normal brain changes that occur during parenthood, but what goes awry in instances of postpartum depression?
Pawluski: A lot of research on depression, including postpartum depression, has focused on the amygdala, a part of the brain responsible for emotional processing. In one study, for example, researchers looked at the amygdala of women who had postpartum depression and others who weren't depressed. When they showed these mothers a picture of an infant, they found the amygdala response is quite a bit higher and more activated in mothers with postpartum depression compared to moms without depression. This means the same brain areas, especially the amygdala, seem to be involved in depression in general, including postpartum depression. However, how the amygdala responds and functions in moms with postpartum depression can be quite different. We need to investigate this further because understanding these functional differences in parental brains will help us develop targeted treatments.
Spotlight: The amygdala
Research has shown certain regions of the brain — amygdala, thalamus, and hippocampus — play a key role in depression. The amygdala, for example, is important because it regulates emotions like happiness, fear, anxiety, and anger. Studies have found that the amygdala of people experiencing depression is extremely active and hyper responsive compared to the amgydala of individuals without depression.
What are some of the biggest risk factors for postpartum depression, and what credible resources do you recommend to new parents?
Pawluski: There's a lot going on, not just physically but also psychologically and socially, from pregnancy to the postpartum period. And while this transition is tough, several risk factors can further increase your likelihood of mental illness during this period. These risk factors include having a history of anxiety or depression or a diagnosis of bipolar disorder or another mental illness. We also know that socio-economic minorities and those who've experienced intimate partner violence are at high risk of postpartum depression.
All of these factors tie in with biology. You don't just have a mental illness out of the blue or without a biological component. So, you may have a tendency toward one because you have a family member who also has a mental illness. It could be how you manage stress. Sometimes, we have control over some of those factors and can lower our risk by, for example, learning to manage stress.
A great resource mentioned in a book by maternal mental health expert Karen Kleiman is the acronym S.E.L.F. This means checking in with yourself by looking at your sleep, exercise, laughter or enjoyment, and food and nutrition. Another important source of support during this time could be Postpartum Support International. This organization has a directory of perinatal mental health professionals who can help if your healthcare provider isn't perinatal-focused or hasn't kept up with the scientific literature.
Source: Dropping the Baby and Other Scary Thoughts: Breaking the Cycle of Unwanted Thoughts in Motherhood by Karen Kleiman and Amy Wenzel
The Food and Drug Administration (FDA) recently approved a new oral medication for postpartum depression, Zurzuvae (zuranolone). How does the medication work?
Pawluski: I've known and followed the work of the researchers behind this drug for a few years, and they've also been active with research on Zulresso (brexanolone), an intravenous (IV) treatment for postpartum depression that came out a couple of years ago. However, IV infusions are quite expensive, so the researchers have been working on an oral treatment, which has just been approved. Essentially, Zurzuvae works by acting on the GABA receptors in the brain. It's able to help normalize brain activity and alleviate symptoms of depression.
Calming chemical
GABA (Gamma-aminobutyric acid) is a brain chemical that inhibits communication between neurons. It decreases activity in the nervous system and regulates emotions like anxiety, fear, and stress. This has a soothing effect when brain circuits are overly excited due to anxiety and depression.
Infographic References
1) Hoekzema, E., Barba-Müller, E., Pozzobon, C. et al. Pregnancy leads to long-lasting changes in human brain structure. Nat Neurosci 20, 287–296 (2017).
2) McCormack, C.Callaghan, B.L.Pawluski, J.L. It’s Time to Rebrand “Mommy Brain”. JAMA Neurol.2023;80(4):335–336.
3) Carmona, S., Martínez-García, M., Paternina-Die, M., et al. Pregnancy and adolescence entail similar neuroanatomical adaptations: A comparative analysis of cerebral morphometric changes. Hum Brain Mapp. 2019 May;40(7):2143-2152. doi: 10.1002/hbm.24513.
4) Sanders, L., "Pregnancy linked to long-term changes in mom's brain." Science News. 2016 Dec
5) Martínez-García, M., , First-time fathers show longitudinal gray matter cortical volume reductions: evidence from two international samples. Cerebral Cortex, 2023 April;33(7): 4156–4163.