Apr 02, 2024, 4:00 am UTC
4 min
Created by
What is Lewy body dementia (LBD) —and why should women care about it?
There’s more than one cause of dementia that can affect women as they age.
Lewy body dementia (LBD) is a term that might not be as familiar as Alzheimer's, but it is a condition that deserves just as much attention. This neurodegenerative disorder affects thinking, memory, movement, and can significantly alter behavior and mood.
But it is difficult to diagnose—often confirmed only by autopsy after a person’s death. That was the case for comedian Robin Williams, who died by suicide in 2014. Williams had been diagnosed with Parkinson’s a few months before his death. According to his wife, he initially struggled with seemingly unrelated symptoms that would come and go, including sleeplessness, a poor sense of smell, and a slight tremor in his left hand. Over 10 months, he developed extreme anxiety, paranoia, delusions, problems with memory, continuous tremor and a shuffling gait.
The prevalence of Lewy body dementia appears to be higher in men than women, but not all studies agree on that. What's clearer is that the condition is often misdiagnosed or undiagnosed in women because women don’t always display the disorder’s core symptoms. Recent research also suggests that the disease might have a unique impact on women.
By understanding the symptoms, diagnosis, and treatment of LBD, as well as the sex- and gender-specific aspects of the disease, we can better support those affected by this challenging condition and their families.
This article covers:
- What is Lewy body dementia (LBD)?
- How does LBD differ from Alzheimer’s and Parkinson’s?
- What are the key symptoms of LBD?
- Do the symptoms of Lewy body dementia differ between men and women?
- How is Lewy body dementia diagnosed and treated?
- What are the sex and gender differences in LBD?
- What are the risk factors for LBD, and can it be prevented?
- What’s happening in LBD research?
- LBD support networks and resources
What is Lewy body dementia (LBD)?
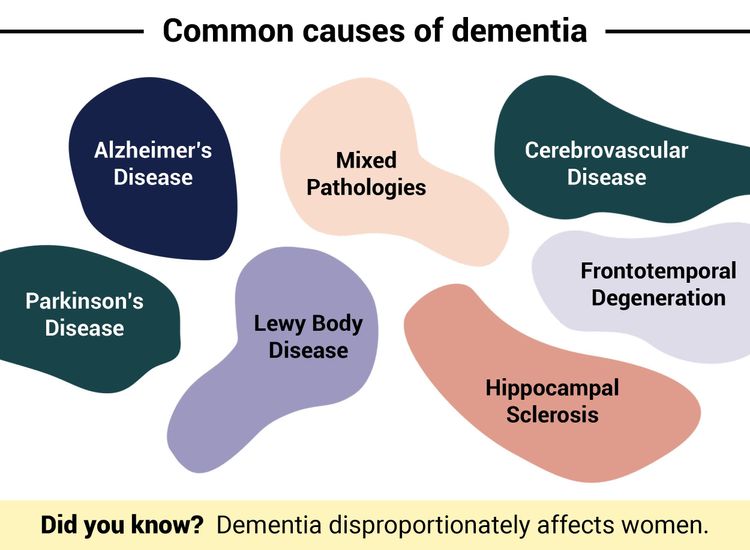
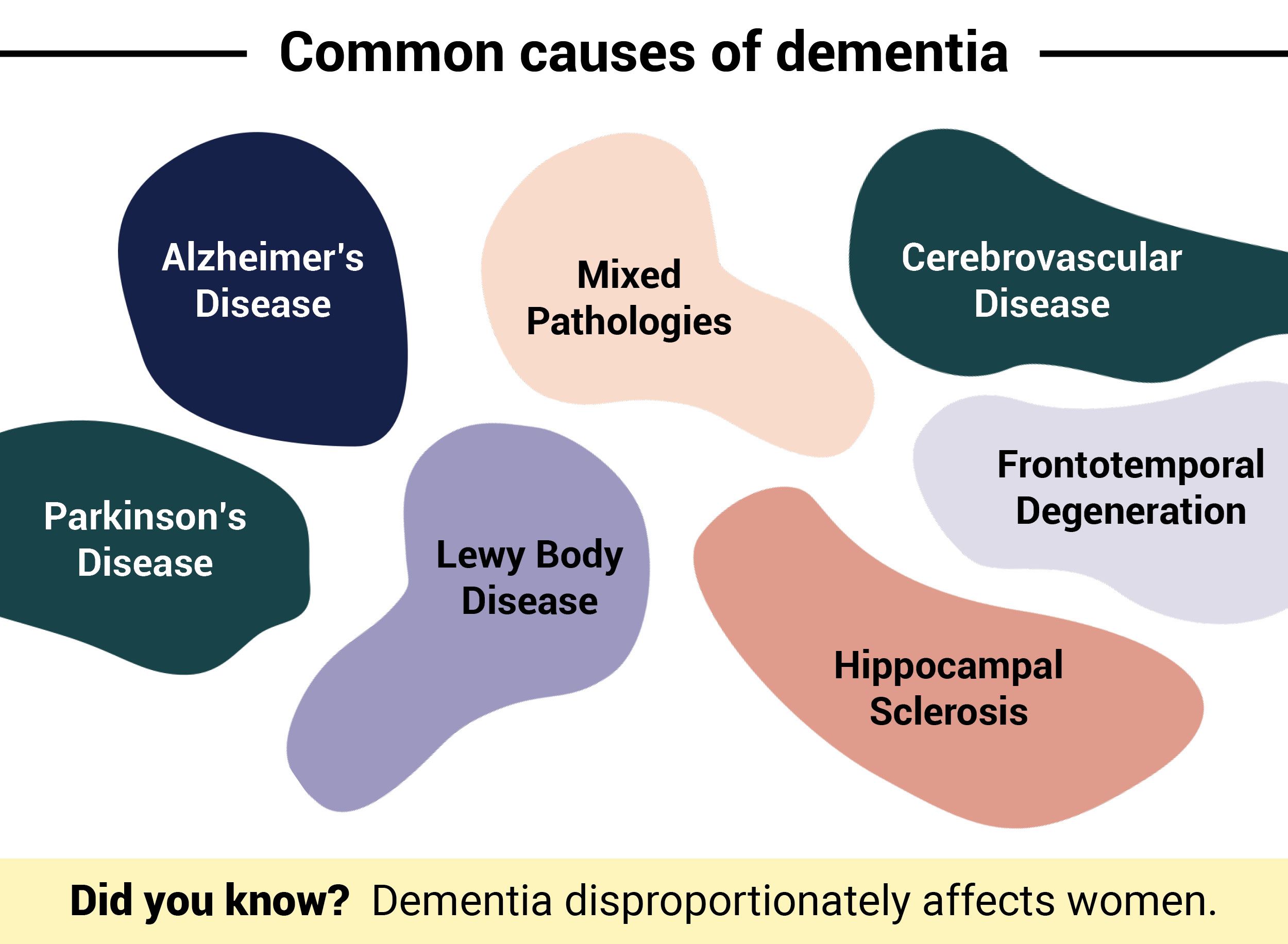
There are many causes of dementia, just like there are many causes of a cough or high blood pressure. Alzheimer’s is the most common cause, followed by Lewy body dementia.
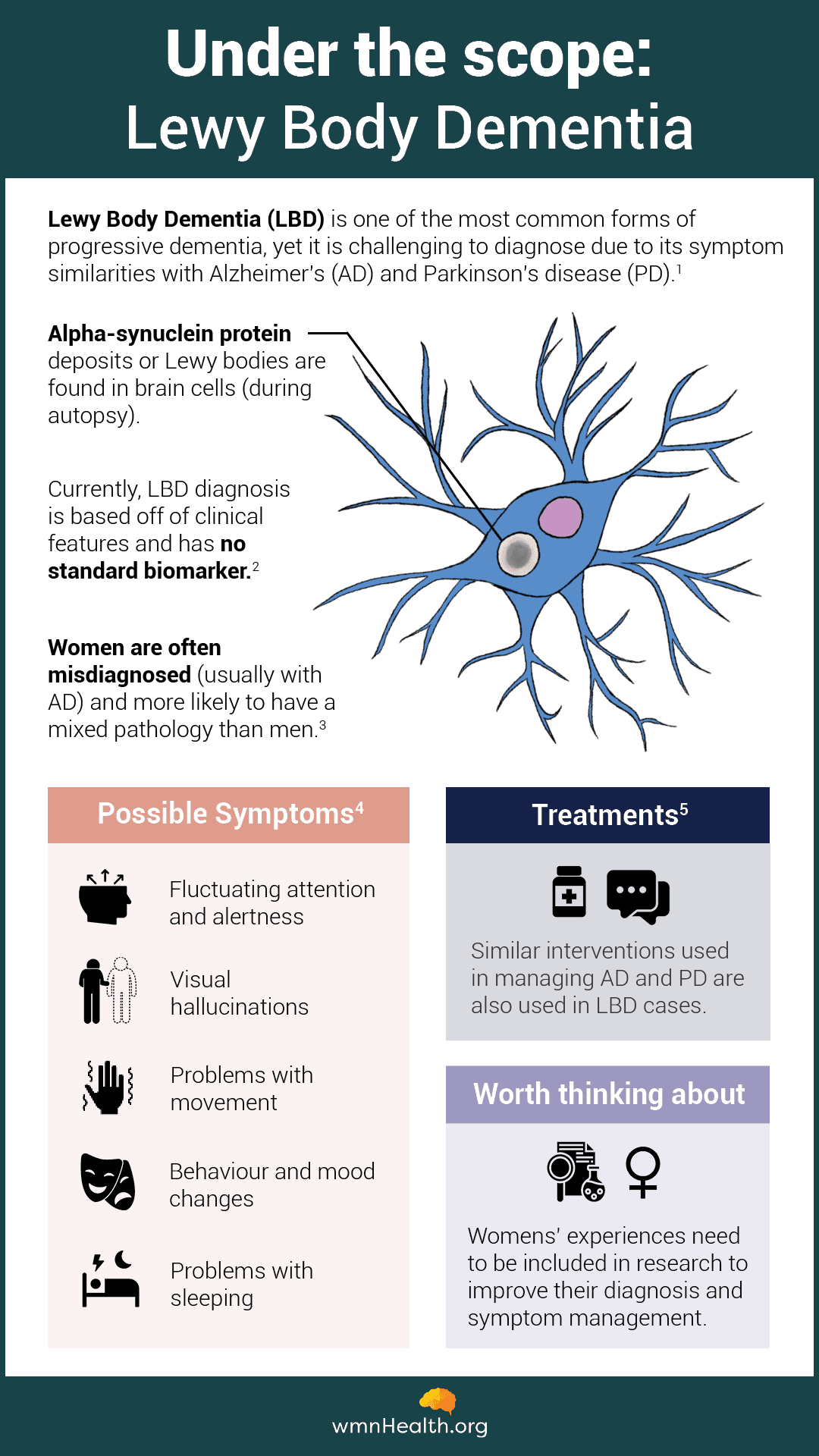
Lewy body dementia is characterized by the presence of abnormal protein deposits, known as Lewy bodies, in the brain. These deposits cause brain cells to degenerate and die, leading to a decline in cognitive, physical, and emotional functions. The symptoms of LBD can be challenging to diagnose because they overlap with those of other more well-known diseases like Alzheimer's and Parkinson's.
Lewy body diseases
Lewy bodies can be seen under the microscope within nerve cells. They consist of deposits of abnormally folded alpha-synuclein, the protein that also builds up in the brains of people with Parkinson’s. As a result, both Parkinson’s and Lewy body dementia are considered “Lewy body diseases.” Lewy bodies disrupt chemical signaling in the brain, altering the neuronal pathways that depend on those signals.
 Infographic by Cat Lau. (References below.)
Infographic by Cat Lau. (References below.)How does Lewy body dementia differ from Alzheimer’s and Parkinson’s?
Lewy body dementia shares features with Alzheimer’s and Parkinson’s, but there are also key differences. For example, people living with Alzheimer’s and Lewy body dementia experience cognitive impairment. However, in Alzheimer’s, people are most likely to have memory issues. In Lewy body dementia, people tend to struggle with executive functions like attention and decision-making, as well as visuospatial processing. In Parkinson’s disease, cognitive impairment tends to occur much later than in Lewy body dementia, where it is usually the defining characteristic. Essentially, a person is diagnosed with Parkinson’s or Lewy body disease, depending on which symptoms present first.
 Infographic by Cat Lau.
Infographic by Cat Lau.What are the key symptoms of Lewy body dementia?
The symptoms of Lewy body dementia are diverse and can vary significantly from person to person. However, some common symptoms include cognitive fluctuations, visual hallucinations, and Parkinsonian movement problems. Cognitive fluctuations can manifest as variations in attention and alertness, while visual hallucinations can be vivid and detailed. Parkinsonian symptoms might include stiffness and difficulty with movement.
Other symptoms can include sleep disturbances, including Rapid eye movement behavior disorder (RBD), behavioral and mood changes, and autonomic dysfunction, which affects the automatic functions of the body, such as blood pressure and digestion.
Rapid eye movement (REM) sleep behavioral disorder
Rapid eye movement (REM) sleep is the stage when we’re dreaming. It is characterized by quick eye movement, relaxed muscles, irregular breathing, elevated heart rate, and increased brain activity. In REM sleep behavioral disorder (RBD), people don’t experience the paralysis normally associated with REM sleep. Instead, they act out their dreams and may shout, punch, kick, or flail in their sleep. RBD has a variety of causes, including Lewy body dementia, sleep apnea, and medications. If you or a loved one develops RBD, you should talk to your doctor about it.
Do the symptoms of Lewy body dementia differ between men and women?
The symptoms of Lewy body dementia are generally milder in women than in men. However, women display fewer of the common symptoms associated with the disease, such as Parkinsonian movement problems. As a result, they tend to be diagnosed later than men, and therefore have more advanced symptoms at the time of diagnosis. Researchers are just beginning to investigate the sex and gender differences associated with Lewy body dementia, including how symptoms vary and how the disease progresses.
How is Lewy body dementia diagnosed and treated?
Diagnosing LBD can be complex because so many of its symptoms overlap with other conditions, especially Parkinson's and Alzheimer's. Furthermore, there is no single test for the disease. Diagnosis often requires a comprehensive evaluation that includes medical history, physical and neurological examinations, and sometimes brain imaging tests, which help doctors determine which brain structures are involved.
There is no cure for LBD, therefore treatment focuses on managing symptoms. This can include medication to help with movement problems or mood disorders, as well as non-pharmacological approaches like physical therapy and cognitive exercises.
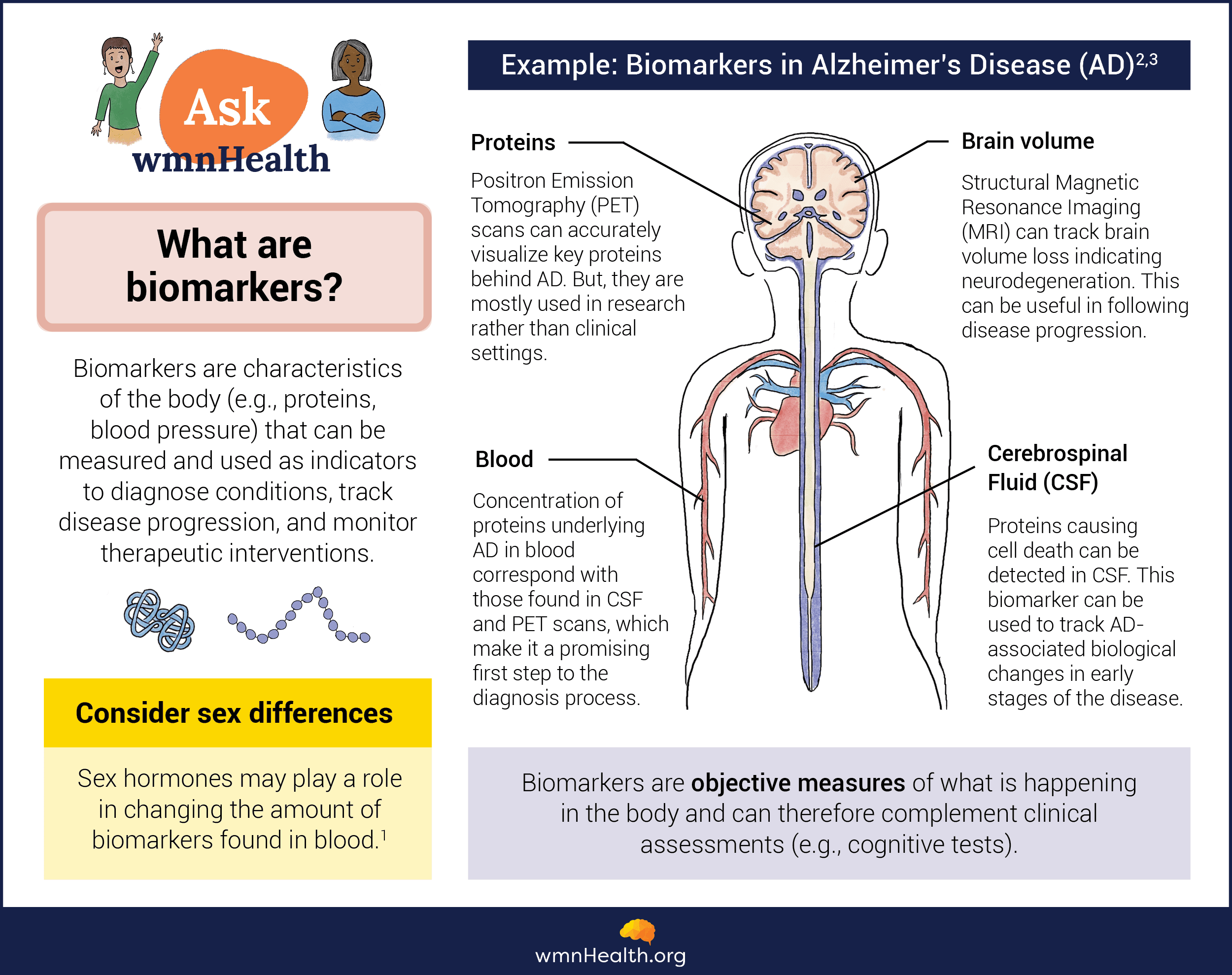
Biomarkers for Lewy body dementia
The search is on for biomarkers—objective measurements of the body in health or disease—that can help doctors diagnose Lewy body dementia more quickly and accurately. Biomarkers for LBD could help detect the condition early and, by distinguishing it from Alzheimer's and Parkinson's, lead to more effective treatment and care. Scientists are currently evaluating potential protein biomarkers in the blood or in the cerebrospinal fluid that surrounds the brain and spinal cord. Another category is imaging biomarkers, which use technologies like MRI and EEG during sleep, to visualize structural and functional changes in the nervous system. Skin biopsies, which can be tested for the presence of abnormal alpha-synuclein deposits, also show promise for detecting Parkinson's and Lewy body dementia long before symptoms appear.
 Infographic by Cat Lau. (References below.)
Infographic by Cat Lau. (References below.)What are the sex and gender differences in LBD?
Studies on sex and gender differences in Lewy body dementia are still few and far between. However, they have indicated that females with LBD might experience a faster progression of the disease compared to men. This could be due to biological differences, such as hormonal changes, or social factors, like differences in caregiving roles. Additionally, females might have different responses to medications used to treat LBD, necessitating a sex-sensitive approach to treatment.
What are the risk factors for Lewy body dementia, and can it be prevented?
The main risk factor for Lewy body dementia is age, just as it is for Alzheimer’s. Other known risk factors include: Parkinson's disease and REM sleep behavior disorder. There is not a clear genetic basis for Lewy body dementia, but having a family member with this condition does slightly increase a person's risk.
While the exact causes of Lewy body dementia are not fully understood, research suggests that lifestyle factors might play a role in reducing the risk of developing LBD. According to Dr. Philip Tipton, a neurologist at the Mayo Clinic in Jacksonville, Florida, the following lifestyle modifications may help prevent Lewy body dementia as well as other neurodegenerative diseases:
- Cognitive exercise – focus on challenging yourself to learn a new skill.
- Social exercise – regular engagement with others.
- Aerobic exercise – getting your heart rate up.
What’s happening in Lewy body research?
Researchers are exploring new treatment options, diagnostic tools, and potential risk factors for Lewy body dementia. A variety of clinical studies are underway to test the effectiveness of new medications and interventions. Participating in research studies can provide access to cutting-edge treatments and contribute to the collective knowledge about Lewy body dementia, including sex and gender differences.
LBD support networks and resources
Living with Lewy body dementia can be challenging, not only for the individuals diagnosed with the condition but also for their families and caregivers. Support networks and resources play a vital role in providing information, emotional support, and practical assistance to those affected by LBD.
Local and national organizations such as the Lewy Body Dementia Association States and Canadian Lewy Body Dementia Information often offer helplines, support groups, educational materials, and research opportunities. These resources can help individuals navigate the complexities of LBD, access specialized care, and connect with others who understand their experiences.
- Lewy Body Dementia Association (USA)
- Canadian Lewy Body Dementia Information
- Lewy Body Dementia Canada
- The Lewy Body Society (United Kingdom)
- National Institute of Neurological Disorders and Stroke: Lewy Body Dementia
Infographic References
Lewy body dementia
- What Is Lewy Body Dementia? Causes, Symptoms, and Treatments, The National Institute on Aging. (Accessed March 20, 2024)
- Diagnosis and Prognosis: How is LBD diagnosed? Lewy body Dementia Association (Accessed March 20, 2024)
- Bayram, E., Reho, P., Litvan, I. et al. Genetic analysis of the X chromosome in people with Lewy body dementia nominates new risk loci. npj Parkinsons Dis. 10, 39 (2024).
- Symptoms, Lewy body Dementia Association (Accessed March 20, 2024)
- Treatment Options, Lewy body Dementia Association (Accessed March 20, 2024)
What are biomarkers?
- Sex differences in biomarkers impact clinical testing, Women's Health Research Institute (accessed January 23, 2024)
- Dubois, B., von Arnim, C.A.F., Burnie, N. et al. Biomarkers in Alzheimer’s disease: role in early and differential diagnosis and recognition of atypical variants. Alz Res Therapy 15, 175 (2023).
- Klyucherev, T.O., Olszewski, P., Shalimova, A.A. et al. Advances in the development of new biomarkers for Alzheimer’s disease. Transl Neurodegener 11, 25 (2022).