Nov 29, 2023, 5:00 am UTC
6 min
Created by
Beyond Statistics: The impact of neurodegenerative diseases on women
In this article, we will cover:
The first person diagnosed with Alzheimer’s disease (AD), the most common form of dementia, was a woman. The odds were in her favor. Females are disproportionately affected by the disease, so much so that today, it is widely recognized that about two-thirds of people with Alzheimer’s disease worldwide are female.
AD is a neurodegenerative disease — a condition characterized by the progressive degeneration or death of nerve cells in the brain or peripheral nervous system. Other common examples are Parkinson’s disease, amyotrophic lateral sclerosis (ALS), Huntington’s disease, and multiple sclerosis (MS). These debilitating diseases result in the gradual loss of cognitive function, motor skills, or both. Specific treatments can relieve some of the physical or psychological symptoms associated with neurodegenerative diseases. But they are currently irreversible, incurable, and far too often a death sentence.
Scientists don’t understand why Alzheimer’s affects more females than males. The same is true for MS, where females with the disease outnumber males approximately three to one. In Huntington’s, where females and males have an equal risk of developing the disease, symptoms appear more severe in females than males. The question is, why?
The answers aren't clear-cut. These conditions are complex and multifactorial. For example, the likelihood of developing a neurodegenerative disease increases dramatically with age — and globally, females outlive males by about 5 years. Genetic, hormonal, lifestyle factors, and even gender inequality likely also play a role in neurodegenerative diseases and how they affect men and women. Also, most brain researchers don't study sex and gender differences. They can't answer questions they aren't asking.
That is beginning to change — and not a moment too soon. According to the WHO, the number of people living with dementia is expected to rise from 55 million in 2019 to 139 million in 2050 as the population ages. Parkinson’s and MS are also on the rise globally, meaning millions more men and women will be living with neurodegenerative diseases. Research is urgently needed to understand how sex and gender influence disease risk, symptoms, and trajectories — and to develop therapies that are effective for everyone.
In this article, we delve into neurodegenerative diseases, explore their effects on women, and why understanding these nuances is crucial.
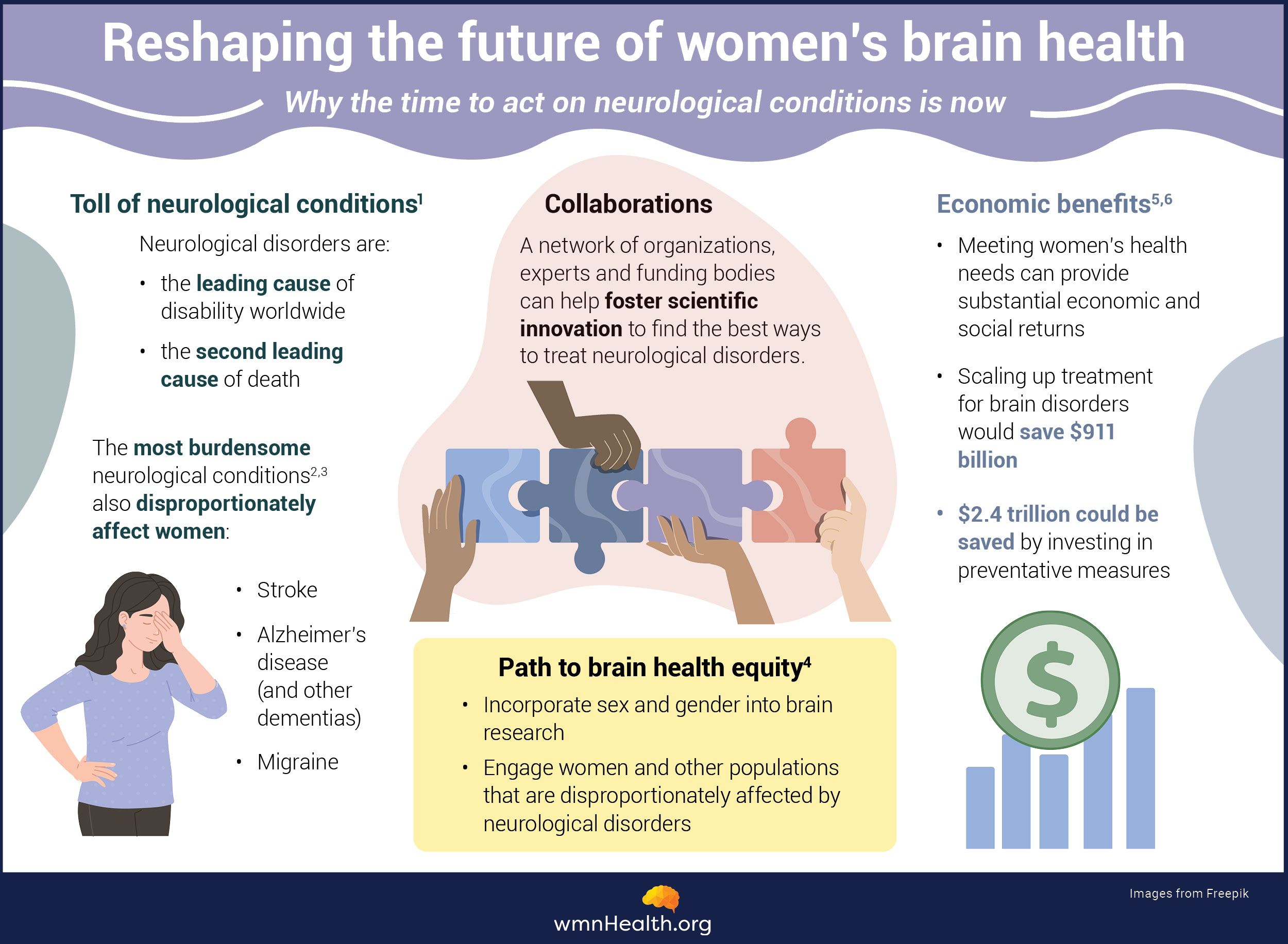 Infographic by Cat Lau. (References below.)
Infographic by Cat Lau. (References below.)What are neurodegenerative diseases?
Neurodegenerative diseases involve the progressive degeneration of nerve cells, leading to cognitive decline and motor dysfunction. Some, like Alzheimer's, primarily affect nerve cells in the brain responsible for cognition, including memory and reasoning. Others, like ALS, primarily cause movement difficulties due to the progressive loss of motor neurons controlling voluntary muscles. Demyelinating diseases like multiple sclerosis are caused by the loss of cells that act like insulation and facilitate the transmission of signals within the nervous system.
Common neurodegenerative diseases include:
- Alzheimer’s disease
- Parkinson’s disease
- Amyotrophic lateral sclerosis (ALS)
- Huntington’s disease
- Multiple sclerosis (MS)
Some of the other neurodegenerative spinal muscular atrophy, Friedreich's ataxia, Frontotemporal dementia, prion diseases, and Lewy body dementia.
A note from wmnHealth: Most research has focused on differences related to biological sex (assigned sex) in neurodegenerative diseases and the male-female binary. As a result, little is known about the experiences of transgender, gender-diverse, and non-binary individuals. The terms "men" and "women" are also commonly used in place of "males" and "females," even though the former refers to gender rather than biological sex. This can make it difficult to interpret the results. It also underscores the need for careful design and analysis of research on sex and gender differences.
Why study neurodegenerative disease in women?
Understanding how neurodegenerative diseases manifest differently in women is crucial for effective diagnosis, treatment, and care. Factors such as hormonal influences, genetic predispositions, and societal roles contribute to unique experiences, making sex- and gender-specific research essential.
That first Alzheimer’s patient was Auguste Deter, who lived near Frankfurt, Germany. She wasn’t quite 50 when her dementia symptoms emerged. When Dr. Alois Alzheimer examined her brain after death, he noted it had shrunk in specific areas and contained abnormal deposits. We now know that as neurons are injured and die in Alzheimer’s, certain brain regions shrink. Those deposits, called plaques and tangles, are caused by molecular and cellular changes that disrupt brain circuits and ultimately prove toxic to cells.
Who gets Alzheimer's?
Alzheimer’s is the most common neurodegenerative disease in the world, affecting 1 in 9 people age 65 and older. In the US, about two-thirds of people with AD are female. Older Black Americans and Hispanics are more likely than older White Americans to develop the disease.
In the United States, about two-thirds of people with AD are female.
What are the common symptoms and early signs?
The most common early symptom of AD is short-memory memory impairment caused by damage to the circuits that help lay down memories in the brain's hippocampal region. As the disease progresses, other forms of memory become impaired, as well as executive functions — higher-order mental processes that enable individuals to plan, organize, initiate, and regulate their actions — and problem-solving. People with the disease may have difficulty finding the right words or understanding what other people are saying, difficulty performing previously routine tasks, as well as personality and mood changes.
What do we know about Alzheimer's in women?
Symptoms: Females with Alzheimer's are more likely to experience depression and anxiety than males, according to some studies.
Risk factors: Age is a major reason females more than males have Alzheimer's. However, longevity doesn't explain everything. Genetic, biological, and social reasons are also likely to be at play. For example, various forms of the Apolipoprotein E gene, known as APOE, are associated with Alzheimer's. The APOE4 form appears to affect females differently than males. Perimenopause and the drop in estrogen levels that accompanies it may also raise the risk of Alzheimer's. On the flip side, the use of hormone replacement therapy during the menopausal transition may protect against dementia.
Researchers are beginning to study how the experiences of males and females over a lifetime impact their dementia risk. Some interesting associations have arisen. For example, research has associated work and education with higher cognitive engagement and cognitive reserve — a person's resilience to age- and disease-related brain changes. Historically, women have had less access to mentally stimulating jobs and higher education, which may reduce their cognitive reserve and increase their risk of dementia.
Treatment: There is no cure for Alzheimer's, though two disease-modifying therapies have recently been approved by the FDA. These drugs help prevent the build-up of toxic proteins in the brain and show modest benefits in preventing cognitive decline. Unfortunately, the drugs appear to be less effective in females than males. More research is needed on sex differences in the response to Alzheimer’s therapies.
Who gets Parkinson's?
After Alzheimer’s, Parkinson’s is the second most common neurodegenerative disease. About one million people in the US are living with Parkinson's — a number that is expected to rise to 1.2 million by 2030. Males are at least 1.5 times more likely to have Parkinson's disease than females. However, females have a higher mortality and faster progression of the disease. Males also have earlier disease onset than females.
Females with Parkinson's disease have a higher mortality and faster progression.
What are the common symptoms and early signs?
PD is a progressive disorder that leads to tremors, muscle stiffness, an unsteady gait, and balance and coordination difficulties. There is also an array of non-motor symptoms associated with PD, including depression, apathy, and sleep disorders, which often go unrecognized and untreated, seriously undermining a person’s quality of life. As PD progresses, dopamine-producing neurons die, mainly in a brain region called the striatum. The striatum is involved in motor functions like the initiation of movement and cognitive functions like decision-making and emotional processing, and is responsible for many of the cardinal features of PD. Nerve cell loss also occurs in other parts of the brain.
What do we know about Parkinson's in females?
"Current literature is scarce and conflicting with how this disease affects women. There are currently no expert opinion guidelines on how to manage PD symptoms in [women]," write Dr. Soania Mathur, Kat Hill, and Dr. Kristi LaMonica in a commentary about a research initiative focused on women with PD.
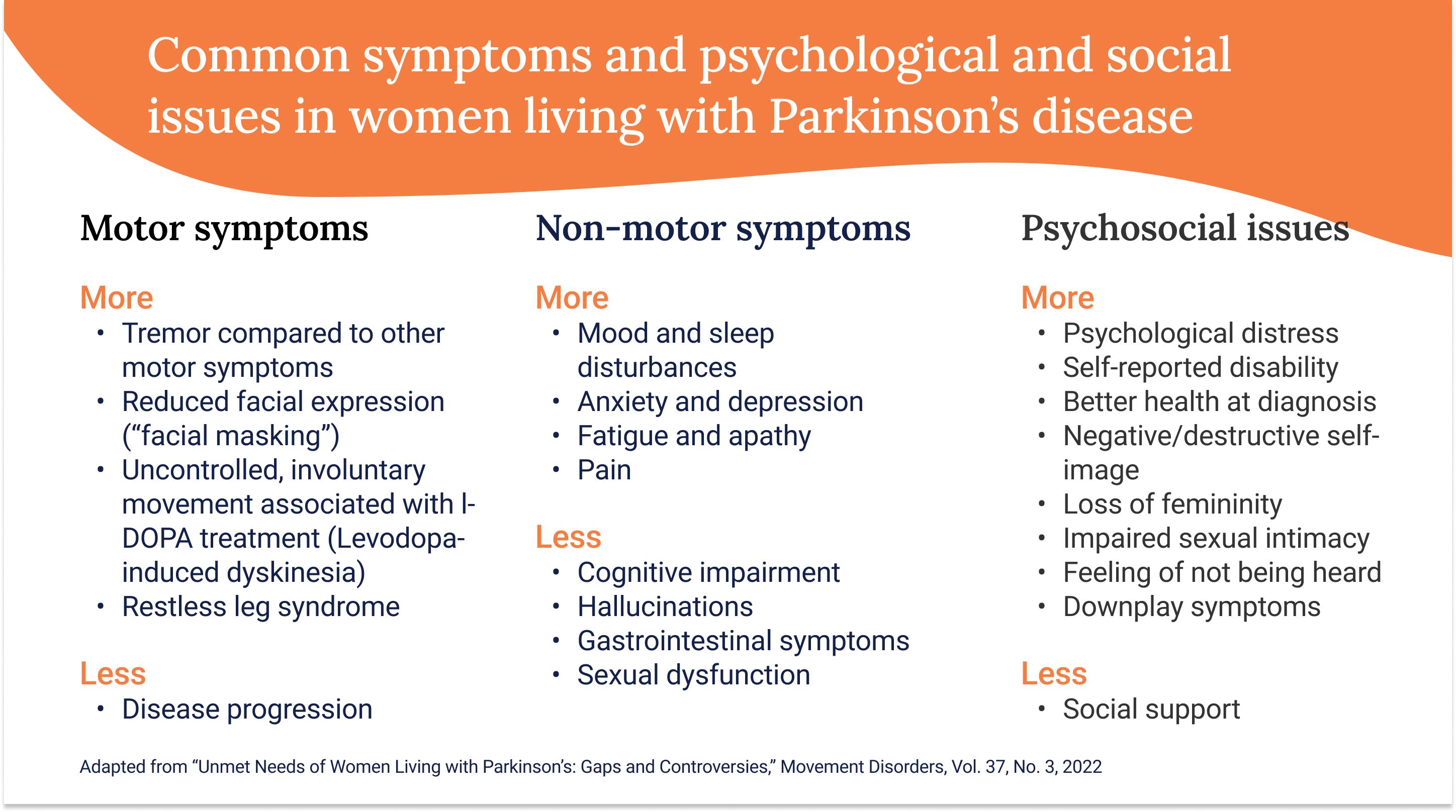
Symptoms: Research suggests females with Parkinson's experience different symptoms, especially non-motor symptoms, and report more side effects and fluctuations in their symptoms than males. Here is a summary.
Risk factors: Estrogen is considered to be a protective factor in the development of PD.
Disease severity and progression: There are sex differences in the severity and progression of Parkinson's. A recent study explored the health factors that may influence PD severity in females. It found that sex-specific experiences are associated with increased severity, including depression, perinatal depression, natural childbirth, vitamin B12 deficiency, and hysterectomy, though further research is needed.
Treatment: There is no cure for PD. Current treatments help manage PD symptoms rather than slow or stop disease progression. There is some evidence that females respond differently to Parkinson's medications and experience more fluctuation in symptoms under treatment than males with the disease.
Who gets ALS?
ALS, also referred to as Lou Gehrig’s disease, is considered a rare disorder, developing in 1.5 to 3 per 100,000 people every year in North America and Europe, though some estimates are now as high as 5 per 100,000. Approximately 80 percent of people die within two to five years of being diagnosed.
It is approximately 20 percent more common in males than females. However, with increasing age, the incidence of ALS (the number of new diagnoses in a year) becomes more equal between men and women.
The onset of ALS tends to be earlier in males compared with females. This may be due to the neuroprotective effects of estrogen.
What are the common symptoms and early signs?
In ALS, the motor neurons carrying signals from the brain and spinal cord to voluntary muscles — those that are under conscious control — gradually deteriorate and die, leading to weakness, atrophy, difficulty with movement and coordination, and paralysis. As the disease progresses, people with ALS lose the ability to walk, talk, eat, swallow, and breathe. Early symptoms include weakness, fatigue, muscle cramping or twitching, stiffness or rigidity.
What do we know about ALS in females?
There has been very little research on sex differences in ALS. However, researchers are evaluating the impact of sex hormones on the immune system in ALS, progression of the disease, and survival.
Symptoms: One study found that females more often complain of bulbar-onset ALS, a form of the disease that affects neurons in the bulbar region of the brainstem and leads to speech, breathing, and swallowing problems. In contrast, males experience onset in the spinal and limb region. Another study on cognitive impairment in ALS — which is experienced by about half of people with the disease — suggested that female patients have twice the risk for developing cognitive dysfunction, specifically problems with executive function, than males.
Risk factors: Age is a major risk factor for ALS, with peak incidence occurring between ages 60 and 75. Sex hormones likely influence ALS risk, too. Specifically, females under 60 account for about five percent of ALS patients, but at menopause and 60 years of age, the number of females with the disease jumps to about 30 percent, according to the U.S. National ALS Registry.
Who gets multiple sclerosis (MS)?
MS is three times more common in females than males, and the typical age of onset is between 20 and 50 years old. Certain types of MS (relapsing MS) are also increasing in females.
Rates of MS vary geographically, with higher rates observed in regions farther from the equator, including Canada. Its prevalence is increasing globally.
What are the common symptoms and early signs?
MS is a chronic autoimmune condition where the immune system mistakenly attacks the myelin — an insulating layer, or sheath, that forms around nerve cells — in the central nervous system. This leads to scar tissue formation (sclerosis) and disrupts communication between the brain and the rest of the body. Symptoms vary widely. The most common are fatigue, visual disturbances, difficulty walking, numbness, and problems with coordination. MS can affect cognitive function, leading to problems with memory, attention, and problem-solving, as well as mood swings, depression, or anxiety, though these symptoms are often overlooked. Unlike Alzheimer's, Parkinson's, and ALS, MS symptoms can vary in severity and may come and go. People with MS often experience periods of relapse (exacerbations or flare-ups) followed by periods of remission, where symptoms improve or stabilize. MS is also rarely fatal. People with the disease have a slightly shorter life expectancy, but the gap is shrinking.
What do we know about MS in females?
Symptoms: Research suggests the symptoms of MS in females and males are similar. However, symptoms may worsen during menstruation as sex hormone levels fluctuate, though results have been inconsistent. More research is needed on the relationship between MS and the menstrual cycle, including on the impact of oral contraceptives on MS symptoms and disease progression.
Research shows that MS seems to be less active during pregnancy, leading to fewer symptoms, followed by a temporary relapse after delivery.
The relationship between MS symptoms and menopause is complex. Studies suggest females may experience less inflammation during menopause but increased disability after menopause, suggesting it may be a turning point in the disease. Little is known about how hormone replacement therapy affects MS.
Risk factors: Scientists do not know what causes MS, though it is likely a combination of genetic and environmental factors. Why MS is more common in females than males is also unclear. Research suggests female sex hormones, vitamin D, inflammatory processes, and obesity may play a role.
Treatment: There is no cure for MS, but there are numerous disease-modifying therapies that reduce future relapse, disability, and damage to the nervous system in the form of scar tissue. Research suggests MS therapies are equally effective in males and females.
Where can women with neurodegenerative diseases get more information?
Alzheimer's disease
- Women and Alzheimer's (Alzheimer's Association)
- The Women's Alzheimer's Movement
- Women Against Alzheimer's (Us Against Alzheimer's)
- Women's Brain Health Initiative
Parkinson's disease
- Women and Parkinson’s Initiative (PD Avengers)
- Women and PD (Parkinson's Foundation)
- Unshakeable MD
Amyotrophic lateral sclerosis
Multiple sclerosis
- Women Living with MS (National Multiple Sclerosis Society)
- Women's Health and MS (MS Canada)
Infographic References
- Feigen, VL et al. The global burden of neurological disorders: translating evidence into policy. Lancet Neuro. 2020;19(3):255-265.
- Women's health research lacks funding - these charts show how. Nature News. (Accessed November 20, 2023.
- GBD 2017 U.S. Neurological Disorders Collaborators. Burden of Neurological Disorders Across the U.S. From 1990-2017: A Global Burden of Disease Study. JAMA Neurol. 2021;78(2):165–176.
- UCLA Health researcher says brain health equity requires ‘paradigm shift’ in research practices. UCLAHealth.org (Accessed November 20, 2023)
- A united front against the global brain health emergency. Politico. (Accessed November 20, 2023)
- Investing in the health of girls and women: a best buy for sustainable development. BMJ 2020;369:m1175