
Apr 04, 2024, 4:00 am UTC
4 min
Closing the Gap: Sex-specific biomarkers for Alzheimer's disease
The search is on for a more accurate way to diagnose and guide the treatment of Alzheimer's in women.
Jessica Caldwell, Director of the Women’s Alzheimer’s Movement Prevention Center at the Cleveland Clinic, has said it before and she’ll say it again: “At its core, Alzheimer’s is a women’s health issue.”
What’s behind her assertion? About two-thirds of people living with Alzheimer’s, the most common form of dementia, are female. And while females are generally diagnosed with the condition later than males, they tend to face a steeper cognitive decline.
“To address it,” according to Caldwell, “we must understand how biological sex contributes to the underpinnings of this disease.”
Scientists are beginning to pinpoint biological changes that are sex-specific and may account for why the disease plays out differently in women. For example, researchers at the Cleveland Clinic have found evidence that the immune system may play a bigger role in Alzheimer’s disease in females than males. Specifically, they pinpointed a set of proteins that are present at much higher levels in the blood of females with Alzheimer’s compared with males. The proteins are all involved in the immune response, and could serve as a biological signature, or biomarker, of the disease in women.
Sex-specific biomarkers are biological indicators or measurable characteristics that differ between males and females. Examples may include hormone levels (such as estrogen), gene expression patterns, metabolites, or specific proteins that are more prevalent or active in one sex compared to the other.
Today, scientists worldwide are searching for and validating biomarkers of neurodegenerative diseases in the skin, blood, cerebrospinal fluid (CSF), eyes, brain and elsewhere. While these discoveries are promising, there’s an urgent need for sex-specific biomarkers that will ensure Alzheimer’s can be accurately diagnosed and effectively treated in women as well as men. After all, if the biological mechanisms driving the disease are different in females and males, the biomarkers may be, too.
What are biomarkers—and why are they important?
Biomarkers are ways to measure and monitor disease. For neurodegenerative diseases, the most common biomarker categories are blood, CSF, and imaging. For example, if a physician suspects a person has Alzheimer’s disease, they may corroborate their diagnosis by looking for the accumulation of protein fragments known as beta-amyloid and tau in the blood, CSF, or brain.
Biomarkers hold the key to detecting Alzheimer’s early, when it is possible to intervene and slow the inevitable cognitive decline as the disease progresses. Biomarkers are also critical to developing effective treatments because they help researchers identify the biological mechanisms driving the disease in a given individual and monitor whether a treatment is having an impact on those mechanisms.
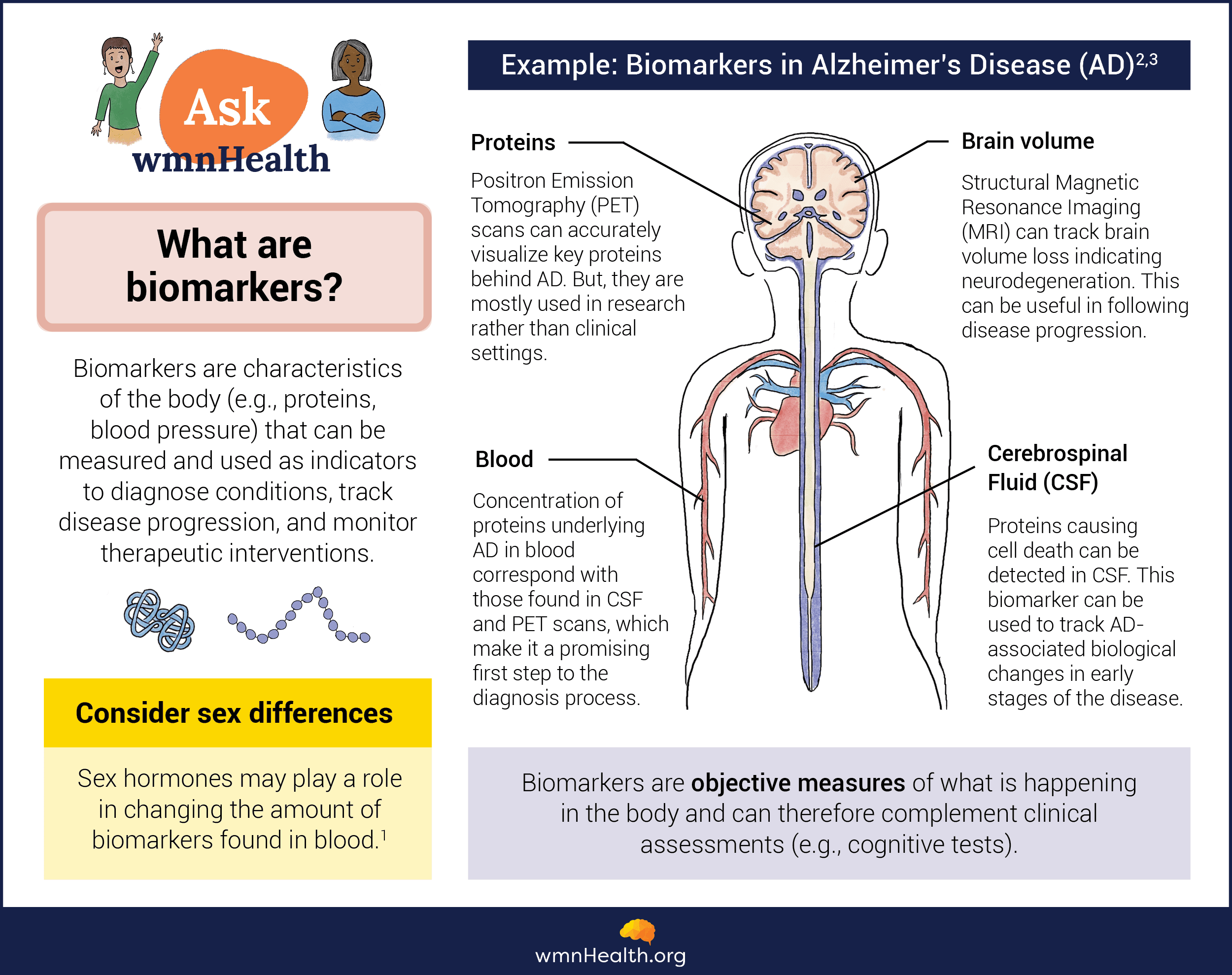 Infographic by Cat Lau. (References below.)
Infographic by Cat Lau. (References below.)
How is Alzheimer’s disease different in women?
The hallmark of Alzheimer’s disease is the buildup of amyloid beta and tau protein fragments in the brain. While these two proteins accumulate in the brains of males and females, studies suggest tau is a particularly important component of the disease in females, who tend to accumulate more abnormal tau than males. Researchers suspect tau may be part of the reason Alzheimer’s is more prevalent in women and progresses faster.
However, there are other molecular mechanisms at play that affect females differently, including dysfunctional immune activity and altered metabolism. These mechanisms may magnify the effects of other disease-causing processes and accelerate cognitive decline.
Immune activation: The brain’s of people with Alzheimer’s show signs of chronic inflammation. This may be caused by the activation of non-neuronal cells like microglia that normally clear waste and debris, including amyloid beta. However, research suggest microglia malfunction in Alzheimer’s and contribute to brain inflammation, which causes further damage to neurons.
Altered cellular metabolism: The brain, more than other organs, has high energy needs, requiring a healthy supply of glucose and oxygen. However, in people with Alzheimer’s, research shows a decrease in glucose and energy production.
A recent study found that interactions between the immune system and cell metabolisms may increase the risk of Alzheimer’s and its severity in women.
The search for sex-specific biomarkers for Alzheimer’s
Scientists like the Cleveland Clinic’s Lynn Bekris are looking for sex-specific biomarkers that could transform care for women with the disease. Bekris is leading a new study funded by the Women’s Alzheimer’s Movement (WAM), which aims to determine if there are biomarkers that are highly sensitive and specific to women or men. The study builds on Bekris’ work suggesting inflammatory factors play a role in the early stages of Alzheimer’s disease, especially in women.
Other researchers have also found sex-specific differences in Alzheimer’s, including in the immune response to the disease. For example, a study led by Claudia Cicognola of Lund University in Sweden showed an increase in biomarkers of microglial activation and inflammation in samples of CSF. Microglia are non-neuronal cells that protect neurons from damage and clear cellular debris and other substances from the brain. But they are also involved in the immune response and, when activated, may contribute to brain inflammation.
Sarah Banks and Erin Sundermann, both professors at the University of California, San Diego, are also studying sex-specific biomarkers as part of research programs dedicated to understanding why Alzheimer’s rates are higher in women. They have a particular interest in immune function and neuroinflammation. Women tend to show a more robust immune response than men, which is helpful to stave off infection. But chronic inflammation in the nervous system may enhance the risk of Alzheimer’s and its progression. Banks and Sundermann’s research suggests that women are more vulnerable to the negative effects of neuroinflammation and that tau plays a role in mediating these effects. The researchers are building on this work to identify sex-specific biomarkers that can be used to diagnose women in primary care and to strengthen the search for effective Alzheimer’s treatments.
Infographic References
- Sex differences in biomarkers impact clinical testing, Women's Health Research Institute (accessed January 23, 2024)
- Dubois, B., von Arnim, C.A.F., Burnie, N. et al. Biomarkers in Alzheimer’s disease: role in early and differential diagnosis and recognition of atypical variants. Alz Res Therapy 15, 175 (2023).
- Klyucherev, T.O., Olszewski, P., Shalimova, A.A. et al. Advances in the development of new biomarkers for Alzheimer’s disease. Transl Neurodegener 11, 25 (2022).


