The innate immune system goes back roughly a billion years, when it developed in early animals as an essential response to infection. Since then, as microbes have evolved elaborate mechanisms to evade detection, this complex network of cells, proteins, and tissues has also kept up through constant learning and adaptation.
Perhaps this is why immunologists still have an incomplete picture of how this vast network operates — and what happens when something goes awry.
Multiple sclerosis, or MS, is a chronic illness of the central nervous system that begins as a misfired immune attack. No two people experience the condition in quite the same way. This article explores the three types of MS that broadly describe how the disease progresses and why there is a need to view the condition as a continuum.
What drives MS?
While the exact mechanisms underlying MS are still coming to light, most experts characterize it as an immune-mediated disease — a condition that arises from an abnormal immune response. In this class of diseases, specialized Y-shaped proteins known as antibodies mistakenly attack the body's healthy tissues.
In MS, when the immune system malfunctions, it sends off these disease-fighting cells to destroy the myelin sheath, which facilitates communication between neurons and protects them from damage. Think of this sheath as a layer of fat and protein wrapped snuggly around a slender bundle of nerve fibers carrying signals from the cell's main body.
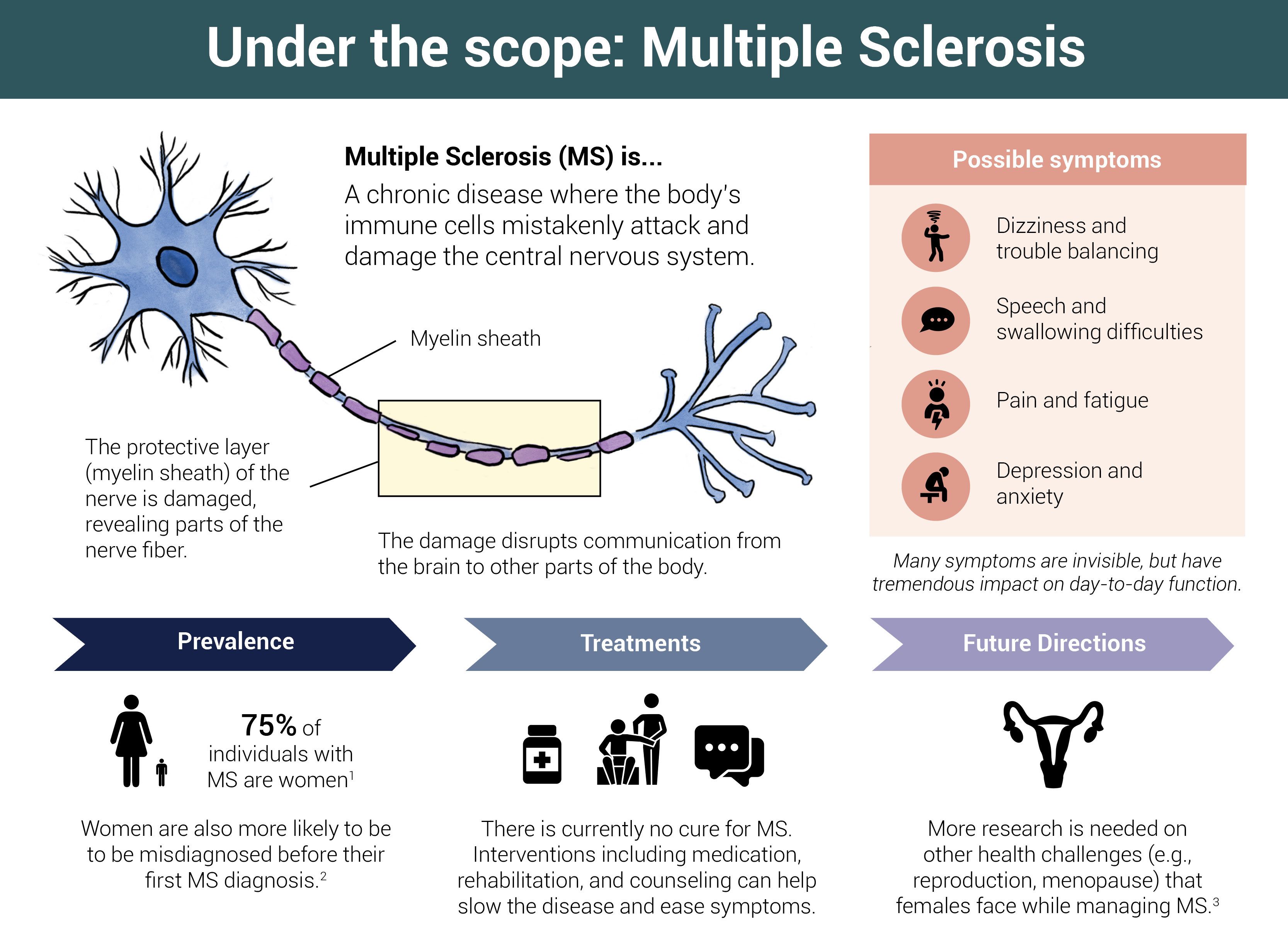 Multiple Sclerosis (MS) is a chronic disease where the body's immune cells mistakenly attack and damage the central nervous system. More than two-thirds of people with MS are female. (Infographic by Cat Lau.)
Multiple Sclerosis (MS) is a chronic disease where the body's immune cells mistakenly attack and damage the central nervous system. More than two-thirds of people with MS are female. (Infographic by Cat Lau.)When this protective wrapping begins to break down — a process called demyelination — these nerve fibers begin to unravel and feather out. This leads to a communication breakdown between nerve cells, affecting a range of cognitive, sensory, and motor functions.
In an attempt to heal the damaged myelin sheath, the body's immune system recruits repair cells called macrophages to the affected areas. These cells contribute to the formation of scar tissue called sclerosis (or lesions), which gives the disease its name. MS lesions can develop in the brain, spinal cord, and optic nerves, and depending on the location of tissue damage, patients with MS experience variability in symptoms — from vision problems to cognitive impairment to movement issues.
 Dark-rimmed spots represent ongoing, "smouldering" inflammation, called chronic active lesions, in an MS patient's brain. Credit: National Institute of Neurological Disorders and Stroke/NIH
Dark-rimmed spots represent ongoing, "smouldering" inflammation, called chronic active lesions, in an MS patient's brain. Credit: National Institute of Neurological Disorders and Stroke/NIHWhat are the different types of MS — and why is there a need to rethink them?
Traditionally, experts have looked at MS as two sides of a coin — one where sudden flare-ups, or relapses, lead to the occurrence of new symptoms or a worsening of old symptoms, and the other where there's a slow progression of symptoms with no distinct attacks.
The relapsing form of MS, also known as relapse-remitting MS (RRMS), is most common, particularly at the time of diagnosis. Patients with this type of MS experience bouts of worsening visual, motor, sensory and other symptoms. These flare-ups can last from days to weeks and vary in severity. The relapse is then followed by a period of recovery, called remission, during which symptoms partly or entirely resolve.
Symptoms of relapse-remitting MS (RRMS), including during flare-ups
- Fatigue
- Stiffness
- Sexual dysfunction
- Bladder and bowel problems
- Challenges with cognition
- Vision problems
Source: MS Society
Studies suggest these relapses in RRMS are due to new or enlarging lesions in the brain. Acute inflammation in and around localized areas, where the myelin sheath has been damaged, can then produce symptoms of MS. Females with the condition are two to three times as likely as males to have this subtype of MS. They also tend to experience symptoms at a younger age, have a higher relapse rate, and report higher levels of depressive symptoms than their male counterparts.
Unfortunately, the unpredictability of MS doesn't end with relapses. The trajectory of the disease is just as relentless and debilitating for people with the second type of MS called primary-progressive MS (PPMS). This, according to experts, is the other face of MS.
Unlike in RRMS, there are no significant fluctuations in symptoms in people with PPMS. Still, predicting how the condition will affect a patient in the long run is extremely tricky — because everyone's symptoms progress at a different rate, and there are currently no tools to deduce how fast the condition will progress or how disabling it will ultimately be.
This rarer form of MS accounts for about 15% of all cases, and the age of onset — when symptoms first start emerging — is almost a decade later than for people with RRMS, who first begin experiencing symptoms between 20 and 40 years of age. This type is more prevalent in males, with females only accounting for 40% of patients with this MS type.
Symptoms of primary-progressive MS (PPMS)
- Dizziness
- Headaches
- Mood changes
- Depression
- Shock-like sensations
- Muscle weakness
Source: Johns Hopkins Medicine
But like most complicated diseases, categorizing MS into distinct disease types is often challenging because the boundaries aren't always so clear. About 25% to 40% of patients with RRMS eventually go on to develop a third type of MS called secondary-progressive MS (SPMS).
Scientists don't have a clear answer yet on how — and why — this transition from relapse-type MS to progressive MS takes place. However, it may depend on how a person's body responds to injury. Some studies suggest it might be due to a higher rate of neurodegeneration — the irreversible loss of neurons — compared to inflammatory changes that drive relapses in RRMS.
Studies that have looked at the relationship between inflammation and neurodegeneration in MS have found that the two likely run hand in hand in all lesions and disease stages. This means progression is a part of MS, with or without relapses.
"We thought if we could silence relapses, the disease would stop," says Dr. Stephen Hauser, a neurologist and researcher at the University of California, San Francisco, who specializes in MS. "And unfortunately, what we learned is that when we silence relapses, we unmask progression, which is very subtle. It's a silent progression present from the beginning, across the MS continuum, but we couldn't see it earlier because of the relapses and remissions."
Early last year, an international panel of experts proposed a new framework for describing MS based on the biological mechanisms of the disease and how they vary from person to person over time. Their recommendation? To move away from the three distinct types of MS that have been used for decades and toward a new system that describes the condition "as a continuum, with contributions from concurrent [disease-causing] processes that vary across individuals and over time."
While this change in thinking would require a better understanding of the underlying biology that drives the condition — and not just how it appears clinically — experts believe this shift would positively impact how patients are cared for. This is because factors like age, biological sex, genes, race, and others can have an enormous impact on how MS manifests and progresses — and they also need to be factored in.
Infographic references
- About MS. MS Canada. https://mscanada.ca/about-ms (Accessed January 17, 2024)
- The Gender Divide: Differences Between Men and Women With MS. MultipleSclerosis.net. https://multiplesclerosis.net/infographic/differences-men-women (Accessed January 17, 2024)
- Ross L, Ng HS, O'Mahony J, Amato MP, Cohen JA, Harnegie MP, Hellwig K, Tintore M, Vukusic S, Marrie RA. Women's Health in Multiple Sclerosis: A Scoping Review. Front Neurol. 2022 Jan 31;12:812147.